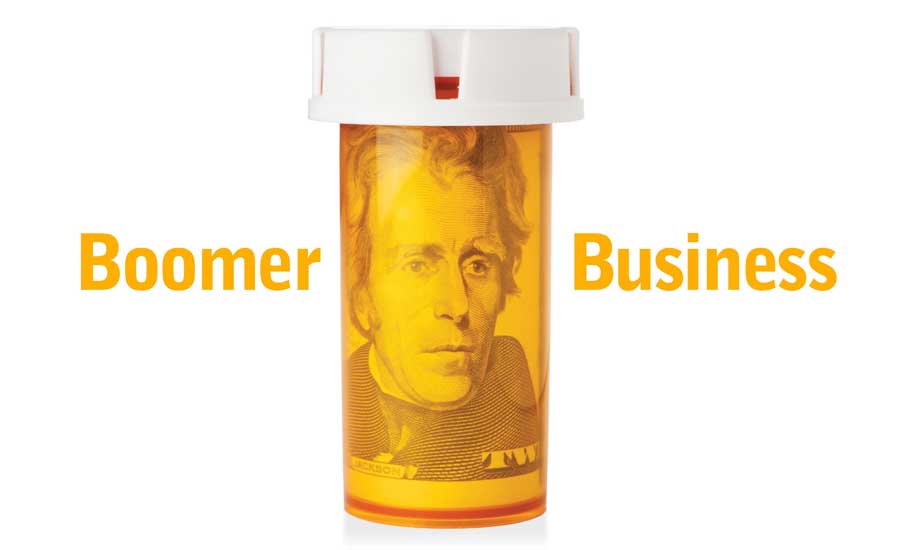
Estimates clearly show that approximately 10,000 Americans become eligible for Medicare benefits every day. This growth should continue at a steady rate for close to two decades. Simultaneously, the race continues for market share in this fast-growing patient segment of the prescription drug industry. With such staggering numbers staring us in the face, independent pharmacists need to take decisive action and stake their claim in this market or risk losing it forever.
The question remains for the Centers for Medicare and Medicaid Services (CMS): How in the world are we going to pay for this? While no one appears to have a complete answer, CMS has manifested its willingness to, in part, address the question by focusing on low-cost medication therapies. In this case, a low-cost medication therapy does not just mean the utilization of low-cost generic drugs. CMS will focus on low-cost medication therapies directed toward those providers that are willing to accept lower costs for dispensing prescription drugs.
If this approach continues, it means your pharmacy will have to accept less money from CMS for dispensing medication therapies, as well as decreased co-payments from Medicare patients. In other words, if you want to have access to this segment of the prescription drug industry at this point in time, it comes at a price.
Effects and influences
The Medicare Part D program has undergone a considerable amount and variety of changes since it went into effect on January 1, 2006. However, in recent years, the plan has been modified in ways that more directly affect independent pharmacies around the nation. Most notably in 2010, the Medicare Part D Prescription Drug Manual was changed to permit patients into preferred networks with varied degrees of cost sharing.
These preferred pharmacies offer Medicare Part D covered drugs at lower out-of-pocket costs than if Medicare patients took their prescriptions to a non-preferred, but in-network pharmacy. Further adding to the confusion is the fact that an individual pharmacy’s status of ‘preferred’ or ‘non-preferred’ may differ within its own sponsorship network.
Even so, Medicare Part D patients have championed the preferred networks. Medicare Part D actuaries and industry insiders believe that 70 percent of the Medicare Part D plans in 2013 will have preferred networks, and they predict an estimated 20 percent of incoming beneficiaries will choose a preferred network plan when they enroll.
The numbers don’t lie. Low-cost is the principle driver for Medicare Part D beneficiaries. Even if they have been going to the same pharmacy for years, the majority of the decisions made by Medicare Part D beneficiaries are ultimately based upon the lowest cost.
Where we are now
There are many different views as to whether CMS’ low-cost medication approach will ultimately succeed in saving the Medicare system. Independent pharmacy has consistently supported the approach that spending an appropriate amount of funds for high quality preventive care through appropriately-monitored medication therapy will improve the health status of Medicare patients and save money overall.
Not only that, preventative-care driven medication therapy has been proven to provide patients with a better quality of life. Various studies have been performed that substantiate this approach. None more often cited than the Ashville Project in North Carolina. Independent pharmacists are uniquely positioned and qualified in the healthcare system to provide extremely effective and high quality professional preventive care services. In short, the pharmacist is in the best place to save the system money through preventive care.
If the independent pharmacist’s position is correct, and yet CMS thinks otherwise and shows no intention of changing its low-cost medication game plan, how are independent pharmacists going to remain a part of the Medicare Part D process?
If we stay on the sideline and complain that the current system doesn’t work, we can only expect things to remain the same. Changes can only be made by participating within the system and proving to the powers-that-be that the preventative-care model is better. That means participating in Medicare Part D preferred networks.
As distasteful as that might sound, we cannot ignore the numbers. Independent pharmacists have to go where the patients are waiting and prove to them that a preventative-care delivery method is better for them. And, that it will lead to a longer and higher quality life.
Action is what matters
Independent pharmacists must establish their place within higher-rated Medicare Part D plans in order to gain a larger share of Medicare Part D patients. They must also work to maintain a consistent five-star rating. One of the major changes in 2013 is that Medicare Part D beneficiaries will be able to change their five-star plan laterally (they can switch to a different five star plan, but cannot choose two or three star plans) if they wish, which would affect performance rates. Patients rate Medicare Part D drug plans every year based on their performance using these star ratings:
- Drug plan customer service
- Member complaints, problems getting services, and improvements in the drug plan’s performance
- Member experience with the drug plan
- Patient safety and accuracy of drug pricing
Since it is illegal for pharmacists to steer Medicare patients to any one plan, pharmacists must perpetuate excellent, personalized customer service practices, and work within plans that maintain the high CMS Medicare Part D star rating. By doing this, independent pharmacy can prove its invaluable position in a healthcare environment that’s ever more focused on cost savings.
Pharmacists must not let CMS confuse low co-pays and ‘cheap drugs’ with the kinds of essential pharmacy services that will provide CMS with the cost savings it seeks. Community pharmacists and their proponents need to incorporate current, detailed empirical data, similar to that brought forth by the Ashville Project, into the Medicare Part D star rating system. By providing evidence, there will be ample proof for CMS that independent pharmacy’s involvement in the cost savings process is not just necessary, but also critical.
This article is by Jim Young, J.D., Director of Third Party Services with PBA Health, a pharmacy services organization based in Kansas City, Mo.